Shoulder Instability Diagnosis and Treatment
Campbell Hogan, Physiotherapist
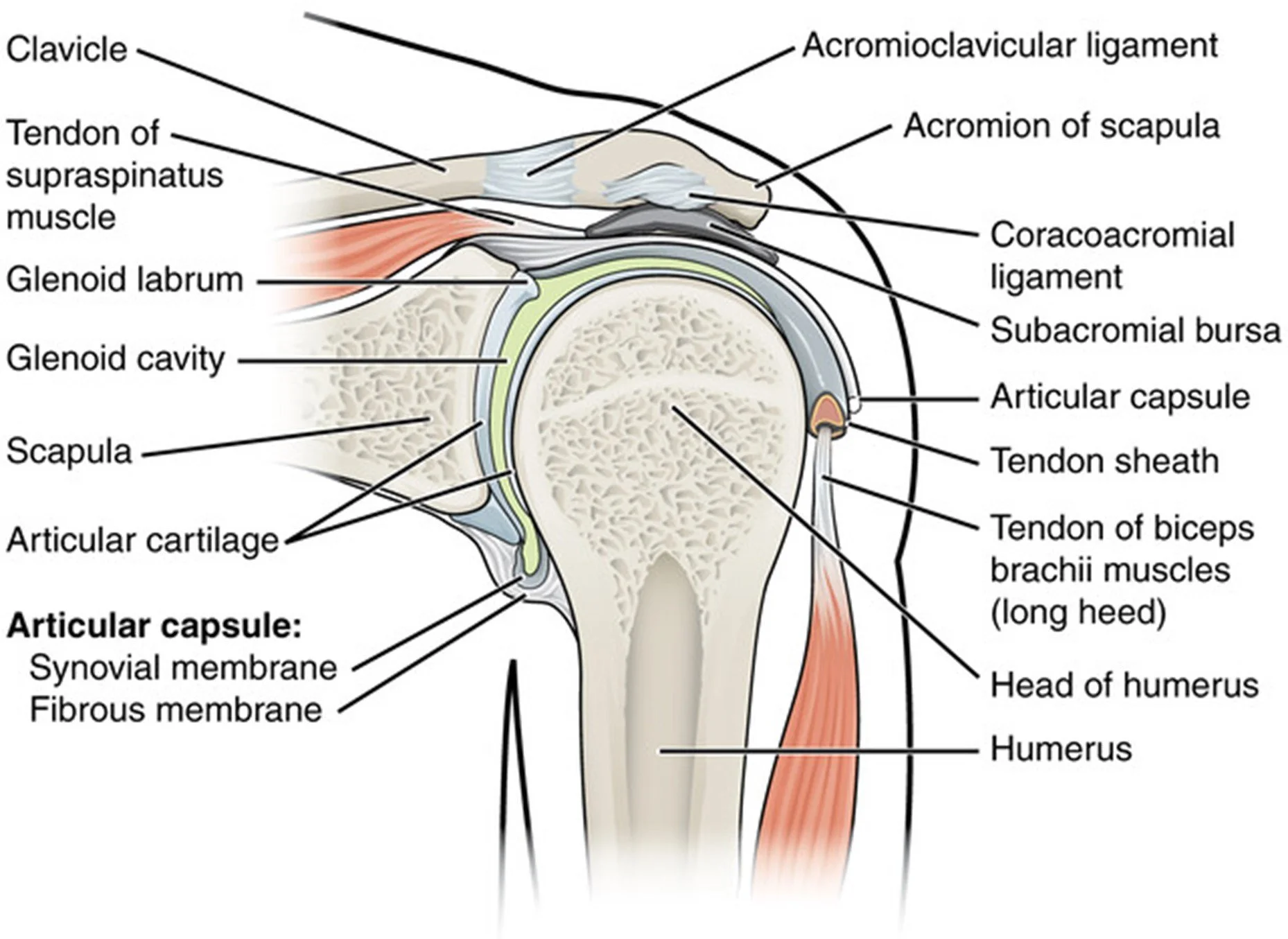
Figure 1: The soft and bony tissues involved in shoulder stability
The shoulder is one of the most fascinating joints in the human body. Playing a pivotal role in upper limb function, the shoulder is highly mobile and can rapidly generate force with very high levels of precision. This is exemplified in the baseball pitch, where the shoulder moves at a rate of 9000°/second to generate a ball speed of up to 170 km/hour (Lewis & Fernández-de-las-Peñas, 2022). The incredible capabilities of the shoulder require a complex stabilisation system comprising of bone, muscles, tendons, ligaments, and the shoulder joint capsule (Figure 1). When there is a disruption or imbalance in this system, shoulder instability can develop leading to pain and reduced shoulder function.
Shoulder instability causes and diagnosis
Shoulder instability can occur when there is an injury to one or more of the tissues that stabilise the shoulder, including the shoulder joint capsule, supporting ligaments, glenoid, labrum and the rotator cuff. Traumatic onset shoulder instability involves sudden high forces placed on the shoulder, for example falling onto the upper limb that results in a dislocation or subluxation. The onset of shoulder instability can also be atraumatic, arising gradually over time with repeated forceful movements at extremes of range, such as those observed in overhead workers or athletes (Woodmass et al., 2019).
The diagnosis of shoulder instability is primarily based on history of the injury and physical assessment. People with shoulder instability often describe shoulder pain, fatigue, instability or a sense of apprehension when using the affected shoulder. Other symptoms can involve mechanical sensations including a clicking or the shoulder "giving way" with movements in one or more directions.
The physical examination often involves the assessment of posture, movement of the shoulder and scapula, strength testing and special tests to determine the presence of instability and if symptoms are modifiable. Imaging, including MRI, CT and Xray, can also play a role in the diagnosis of shoulder instability, and is particularly important when the onset of symptoms is traumatic and involves a dislocation.
Treatment options for shoulder instability
Figure 2: Shrug exercise commonly used in shoulder instability rehabilitation
There are many different treatments available for shoulder instability including taping, bracing, exercise and surgical interventions. Consulting a health professional, such as a physiotherapist, is critical for planning an individualised and effective treatment plan.
For atraumatic instability graded exercise rehabilitation is considered first-line treatment and is effective for up to 80% of people (Noorani et al., 2019). Rehabilitation may include exercises to improve shoulder and scapular motor control, coordination and strength (Figure 2). There are many different exercise programs available for shoulder instability, however, it has been demonstrated that programs that progress in intensity over time and include an initial focus on scapular motor control may be more effective (Warby et al., 2018). Surgical intervention for atraumatic instability is less common but can be considered if there has been limited response to consistent graded exercise rehabilitation for a duration of 6 months.
The management of traumatic instability may involve taping and bracing during the early stages of treatment, followed by progression to a graded exercise rehabilitation program. Early surgical opinion can also be considered in the case of traumatic dislocation and the presence of significant soft tissue or bony injury.
The physiotherapists at Advance Healthcare can assess the nature of your shoulder problem and provide advice on the most effective treatment to support your recovery. Contact info@advancehealthcare.com.au for more information.
References
Lewis, J., & Fernández-de-las-Peñas, C. (2022). The shoulder: theory and practice. Handspring publishing.
Noorani, A., Goldring, M., Jaggi, A., Gibson, J., Rees, J., Bateman, M., Falworth, M., & Brownson, P. (2019). BESS/BOA patient care pathways: Atraumatic shoulder instability. Shoulder & elbow, 11(1), 60-70.
Warby, S. A., Ford, J. J., Hahne, A. J., Watson, L., Balster, S., Lenssen, R., & Pizzari, T. (2018). Comparison of 2 Exercise Rehabilitation Programs for Multidirectional Instability of the Glenohumeral Joint: A Randomized Controlled Trial. Am J Sports Med, 46(1), 87-97. https://doi.org/10.1177/0363546517734508
Woodmass, J. M., Lee, J., Wu, I. T., Desai, V. S., Camp, C. L., Dahm, D. L., & Krych, A. J. (2019). Incidence of posterior shoulder instability and trends in surgical reconstruction: a 22-year population-based study. Journal of shoulder and elbow surgery, 28(4), 611-616.
Campbell completed his Physiotherapy training with research specialisation at Monash University, where he graduated with the highest aggregate marks amongst his peers. For his commitment to learning and achievements during his training, Campbell was awarded the Constance Read Memorial Prize, Eliza McAuley Memorial Prize and the Sir John Monash Medal.